
Cold weather brings with it a host of seasonal discomforts, but for some individuals, exposure to cold temperatures triggers more than just shivers.
Allergy to cold, known medically as cold urticaria, is a rare condition characterized by skin reactions upon exposure to cold temperatures. Understanding its symptoms, causes, and management is crucial for those affected by this condition.
Symptoms of cold urticaria
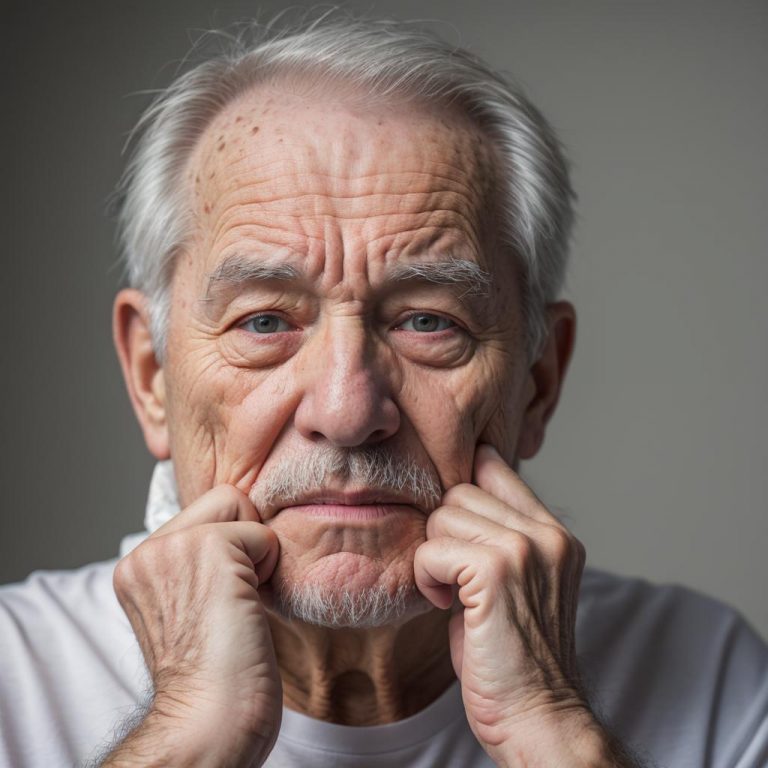
The symptoms of cold urticaria can vary in severity from person to person. Upon exposure to cold air or water, individuals may experience: Red, itchy hives (urticaria) on the skin Swelling of the affected area A burning or stinging sensation Headaches Fatigue Dizziness or fainting in extreme cases These symptoms typically occur within minutes of exposure to cold and can last for several hours.
Causes of cold urticaria
Cold urticaria occurs when the skin reacts abnormally to cold temperatures. While the exact cause is not always clear, it is believed to involve an immune system response triggered by cold exposure. Some potential causes and risk factors include: Genetics: Cold urticaria can run in families, suggesting a genetic predisposition to the condition. Underlying health conditions: Certain autoimmune disorders, such as lupus or hepatitis, may increase the risk of developing cold urticaria. Infections: Viral infections, such as the Epstein-Barr virus, have been linked to the onset of cold urticaria in some cases.
Diagnosis
Diagnosing cold urticaria typically involves a thorough medical history review and physical examination by a healthcare professional. In some cases, additional tests may be conducted, such as: Cold stimulation test: Exposing a small area of the skin to a cold object or ice cube to observe any allergic reaction. Blood tests: To check for underlying conditions or elevated levels of certain antibodies.
Management and treatment
While there is no cure for cold urticaria, several strategies can help manage symptoms and reduce the risk of reactions: Avoiding cold exposure: Minimizing exposure to cold temperatures, especially in windy or wet conditions, can help prevent symptoms. Dressing appropriately: Wearing warm clothing, including gloves, hats, and scarves, can provide a barrier against cold-induced reactions. Antihistamines: Over-the-counter or prescription antihistamine medications can help alleviate itching and reduce the severity of hives. Epinephrine autoinjector: In severe cases where anaphylaxis is a risk, carrying an epinephrine autoinjector and knowing how to use it is essential. Allergist consultation: Working with an allergist or immunologist can help develop a personalized management plan tailored to individual needs. Cold urticaria, or allergy to cold, is a rare but potentially serious condition that can significantly impact an individual’s quality of life. By understanding the symptoms, causes, and management strategies associated with this condition, those affected can take proactive steps to minimize the risk of allergic reactions and lead a more comfortable life, even in chilly weather. If you suspect you may have cold urticaria, it’s essential to seek medical evaluation and guidance for proper diagnosis and management.
Pictures of latex allergy rash: recognizing symptoms and seeking relief
Understanding latex allergy
Latex allergy is a common hypersensitivity reaction to latex, a natural rubber material derived from the sap of the rubber tree. While latex is widely used in various products, such as gloves, condoms, balloons, and medical devices, some individuals may develop an allergic response upon exposure to latex proteins. One of the most noticeable symptoms of latex allergy is the development of a characteristic rash.
Identifying latex allergy rash
The rash associated with latex allergy typically appears shortly after contact with latex-containing products. It can manifest as redness, itching, swelling, and in severe cases, blistering or hives. The rash often occurs in areas that have had direct contact with latex, such as the hands, arms, face, or genital region. The severity of the rash can vary depending on the individual’s sensitivity to latex and the duration of exposure.
Visual representation of latex allergy rash
Pictures of latex allergy rash serve as valuable tools for identifying and understanding this allergic reaction. These images depict the various stages and manifestations of the rash, providing a visual reference for individuals who suspect they may have latex allergy. In many cases, the rash appears as raised, red patches or bumps on the skin, resembling other types of allergic reactions.
Common features of latex allergy rash
While the appearance of latex allergy rash can differ from person to person, several common features may aid in its recognition. These include:
Redness: The affected area often becomes red and inflamed, indicating an inflammatory response to latex exposure.
Itching: Itchiness is a prevalent symptom of latex allergy rash, prompting individuals to scratch the affected area, which can exacerbate the irritation.
Swelling: In some cases, the skin may swell around the rash, leading to discomfort and a feeling of tightness.
Blisters: Severe cases of latex allergy can cause the formation of fluid-filled blisters on the skin, which may rupture and become painful.
Hives: Raised, itchy welts known as hives can develop in response to latex exposure, often appearing suddenly and disappearing within hours.
Seeking relief and treatment
If you suspect you have a latex allergy or experience symptoms of latex allergy rash, it’s essential to seek medical advice promptly. While avoiding latex-containing products is the primary strategy for managing latex allergy, healthcare providers may recommend medications to alleviate symptoms, such as antihistamines or topical corticosteroids to reduce inflammation and itching.
Preventing latex allergy rash
Prevention is key in managing latex allergy and avoiding the associated rash. Strategies for preventing latex allergy rash include:
Avoiding latex-containing products whenever possible, opting for latex-free alternatives.
Using non-latex gloves for tasks that require hand protection, such as cleaning or medical procedures.
Informing healthcare providers, including dentists and surgeons, about latex allergy before undergoing procedures to ensure appropriate precautions are taken.
Wearing a medical alert bracelet or necklace indicating latex allergy to alert others in case of emergencies.
Pictures of latex allergy rash provide valuable insights into this common allergic reaction, aiding in its recognition and management. By familiarizing themselves with the symptoms and visual characteristics of latex allergy rash, individuals can take proactive measures to prevent exposure to latex-containing products and seek appropriate medical care if needed. Remember, early identification and intervention are crucial in managing latex allergy and minimizing the discomfort associated with the rash.
Lips allergy: symptoms, causes, and treatment
Understanding lips allergy
Lips allergy, though often overlooked, can be a bothersome condition affecting many individuals. The skin on the lips is sensitive, making it susceptible to various allergens and irritants. When the lips come into contact with these triggers, they may react with symptoms ranging from mild discomfort to severe swelling and itching.
Symptoms of lips allergy
Identifying a lips allergy can be crucial in managing the condition effectively. Some common symptoms include: Swelling Itching or burning sensation Redness or rash Dryness or chapping Blisters or bumps Peeling or flaking
Potential causes
Understanding the causes of lips allergy can help in avoiding triggers. Here are some common culprits: Cosmetic Products: Lipsticks, lip balms, or lip glosses containing certain ingredients like fragrances, dyes, or preservatives can trigger an allergic reaction. Foods: Certain foods can cause allergic reactions when they come into contact with the lips. Citrus fruits, nuts, and spicy foods are common offenders. Medications: Some medications, particularly those applied topically like lip balms containing medication, can cause allergic reactions. Environmental Factors: Exposure to environmental allergens such as pollen, pet dander, or harsh weather conditions can irritate the lips. Insect Bites or Stings: Insect bites or stings around the lips can cause localized allergic reactions.
Diagnosis and treatment
If you suspect a lips allergy, it’s essential to consult a healthcare professional. They may perform tests to identify the specific allergen causing the reaction. Treatment options may include: Avoidance: Once the allergen is identified, avoiding exposure to it can prevent future allergic reactions. Topical Treatments: Over-the-counter hydrocortisone creams or ointments can help alleviate symptoms like itching and swelling. Antihistamines: Oral antihistamines can be effective in reducing itching and inflammation associated with lips allergy. Moisturizers: Using hypoallergenic lip balms or moisturizers can help soothe dry, chapped lips. Prescription Medications: In severe cases, a healthcare provider may prescribe stronger medications like corticosteroids to control inflammation.
Prevention tips
Taking preventive measures can reduce the risk of experiencing lips allergy: Choose hypoallergenic cosmetic products free from fragrances, dyes, and harsh chemicals. Be cautious when trying new foods or medications, especially if you have a history of allergies. Protect your lips from harsh weather conditions by using lip balms with SPF and covering them in cold or windy weather. Avoid licking your lips, as saliva can exacerbate dryness and irritation. Keep your surroundings clean and free from potential allergens like dust and pet dander. Lips allergy can significantly impact one’s quality of life, causing discomfort and inconvenience. By understanding the symptoms, causes, and treatment options, individuals can effectively manage this condition. If you experience persistent or severe symptoms, seek medical attention promptly to receive appropriate care and relief. Remember, prevention is key in avoiding lips allergy triggers and maintaining healthy, happy lips.
Dog flea allergy: understanding, treating, and preventing
Dog flea allergy, also known as flea allergy dermatitis (FAD), is a common skin condition in dogs caused by an allergic reaction to flea saliva. It affects dogs of all breeds and ages and can cause significant discomfort and distress to the affected animals. Understanding the causes, symptoms, treatment, and prevention strategies for dog flea allergy is crucial for maintaining the health and well-being of our canine companions.
Causes
Flea allergy dermatitis is triggered by an allergic reaction to proteins present in the saliva of fleas. When fleas bite and feed on a dog’s blood, they inject saliva into the skin to prevent blood clotting. In dogs with flea allergy, the immune system reacts excessively to these proteins, leading to inflammation, itching, and skin irritation. Even a single flea bite can trigger a reaction in sensitive dogs.
Symptoms
The symptoms of dog flea allergy primarily manifest as skin irritation and discomfort. Common signs include:
Intense itching, especially around the base of the tail, lower back, abdomen, and hindquarters
Excessive scratching, biting, or licking of the affected areas
Redness, inflammation, and small bumps or scabs on the skin
Hair loss or thinning, particularly in the areas where the dog has been scratching
Secondary skin infections due to scratching and self-trauma
Treatment
Treating dog flea allergy involves addressing both the allergic reaction and eliminating the underlying flea infestation. Treatment options may include:
Topical or oral flea control medications to kill fleas on the dog and prevent future infestations
Medicated shampoos or sprays to soothe irritated skin and reduce inflammation
Antihistamines or corticosteroids to alleviate itching and reduce allergic reactions
Antibiotics or antifungal medications to treat secondary skin infections
Regular grooming and bathing to remove fleas and their eggs from the dog’s coat
Prevention
Preventing flea infestations is key to managing and preventing flea allergy dermatitis in dogs. Here are some preventive measures to consider:
Use year-round flea control products recommended by veterinarians
Regularly vacuum and clean your home, focusing on areas where your dog spends time
Wash your dog’s bedding, toys, and other belongings frequently in hot water
Keep your yard and outdoor areas tidy to minimize flea habitats
Consider environmental flea control methods, such as flea bombs or yard sprays, if infestations occur
Dog flea allergy can significantly impact a dog’s quality of life, causing discomfort, irritation, and skin problems. By understanding the causes, symptoms, treatment options, and preventive measures for flea allergy dermatitis, dog owners can effectively manage the condition and provide relief for their furry friends. Regular flea control, grooming, and vigilant monitoring are essential for keeping dogs healthy and flea-free. If your dog exhibits signs of flea allergy, consult with your veterinarian for proper diagnosis and treatment tailored to your pet’s needs. With proper care and attention, dogs with flea allergy can live comfortable and happy lives.
Kirkland allergy medicine: your comprehensive guide to relief
Dealing with allergies can be a challenging and uncomfortable experience for many individuals. From seasonal allergies to indoor allergens, the symptoms can range from mild irritation to severe discomfort. Fortunately, there are numerous over-the-counter medications available to help alleviate these symptoms, and one popular option is Kirkland Allergy Medicine. In this comprehensive guide, we’ll delve into what Kirkland Allergy Medicine is, how it works, its benefits, potential side effects, and more.
Understanding kirkland allergy medicine
Kirkland Allergy Medicine is a brand of over-the-counter allergy relief medication manufactured by Kirkland Signature, a private label brand owned by Costco Wholesale Corporation. The medication is designed to provide relief from common allergy symptoms such as sneezing, itching, runny nose, and watery eyes. It contains active ingredients that target histamine receptors in the body, helping to reduce the body’s allergic response.
Active ingredients and formulations
Kirkland Allergy Medicine is available in several formulations, including tablets, capsules, and liquid gels. The active ingredients may vary depending on the specific formulation, but the most common ones include: Cetirizine Hydrochloride: This antihistamine works by blocking the action of histamine, a substance in the body that triggers allergic symptoms. Loratadine: Another antihistamine that provides relief from symptoms such as sneezing, itching, and runny nose. Fexofenadine Hydrochloride: Like cetirizine and loratadine, fexofenadine is an antihistamine that helps alleviate allergy symptoms. These active ingredients are non-drowsy formulas, making Kirkland Allergy Medicine suitable for daytime use without causing significant drowsiness.
Benefits of kirkland allergy medicine
There are several benefits to choosing Kirkland Allergy Medicine for your allergy relief needs: Effective Symptom Relief: The active ingredients in Kirkland Allergy Medicine target a wide range of allergy symptoms, providing effective relief for sneezing, itching, nasal congestion, and more. Non-Drowsy Formula: Unlike some other allergy medications, Kirkland Allergy Medicine is formulated to be non-drowsy, allowing you to go about your daily activities without feeling excessively tired or lethargic. Long-Lasting Relief: Many users report that Kirkland Allergy Medicine provides long-lasting relief from allergy symptoms, allowing them to enjoy extended periods of comfort without the need for frequent dosing. Cost-Effective: As a private label brand sold at Costco Wholesale, Kirkland Allergy Medicine often offers cost savings compared to name-brand allergy medications, making it an affordable option for many consumers.
Potential side effects
While Kirkland Allergy Medicine is generally considered safe for most people, some individuals may experience side effects. Common side effects associated with antihistamine medications include: Drowsiness Dry mouth Headache Nausea In rare cases, more serious side effects such as allergic reactions or difficulty breathing may occur. It’s essential to read the product label carefully and follow the recommended dosage instructions to minimize the risk of adverse effects.
Who should avoid kirkland allergy medicine?
While Kirkland Allergy Medicine is safe for most adults and children over the age of six, there are certain groups of people who should avoid using it without consulting a healthcare professional. These include: Individuals with severe liver or kidney disease Pregnant or breastfeeding women Those taking other medications that may interact with antihistamines If you fall into any of these categories or have any underlying health conditions, it’s essential to speak with your doctor before using Kirkland Allergy Medicine or any other over-the-counter medication. In conclusion, Kirkland Allergy Medicine is a popular over-the-counter medication that offers effective relief from common allergy symptoms. With its non-drowsy formula, long-lasting benefits, and cost-effective pricing, it’s a preferred choice for many allergy sufferers. However, like any medication, it’s essential to use Kirkland Allergy Medicine responsibly and consult a healthcare professional if you have any concerns or underlying health conditions. By doing so, you can enjoy the relief you need while minimizing the risk of potential side effects.



